Residency Program
Program Structure and Educational Goals
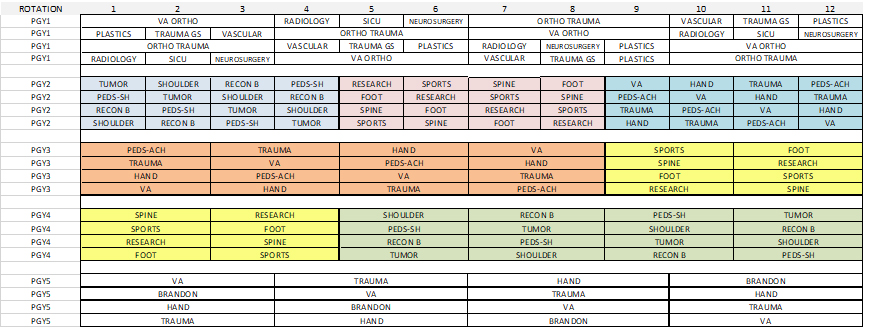
Rotation Level: PGY 1
The first year of orthopaedic surgery residency establishes the critical foundation of both orthopaedic and general surgical knowledge and skills. A strong foundation in patient evaluation, diagnosis, and surgical management sets the tone for continued growth throughout orthopaedic surgical residency and beyond.
Intern year is structured to emphasize hands-on learning in a team setting. Residents are exposed to the breadth of orthopaedics, and will become proficient in settings as diverse as routine outpatient clinic visits to high-energy musculoskeletal injury and polytrauma. Residents learn to manage a large inpatient service, gain efficiency and competence in evaluating emergent and non-emergent consultations, perform bedside procedures and skeletal stabilization, and collaborate in inter-disciplinary care. Senior residents and attending surgeons provide constant guidance and feedback through dedicated conferences, radiology review, and discussion of treatment plans, ensuring appropriate understanding and application of core orthopaedic principles.
Interns participate in a dedicated Skills Lab and Boot Camp led by experienced attending surgeons, occurring weekly for the first 4 weeks. The Skills Labs are based off of the American Board of Orthopaedic Surgery (ABOS) curriculum and include multiple cadaveric dissections to instill the basics of musculoskeletal anatomy, demonstrate and practice appropriate surgical techniques, understand soft tissue handling, and gain familiarity with instrumentation for fracture fixation and arthroplasty. Additionally, the Boot Camp provides a lecture series encompassing the orthopaedic consultation, art of the physical examination, and efficient evaluation of orthopaedic surgical emergencies. Finally, hands-on skills are taught for reduction of long bone fractures and joint dislocations, and correct methods of provisional stabilization (splinting, casting, skeletal traction, etc). In addition to this intensive 8 week curriculum, regular cadaveric anatomy and surgical skills labs continue throughout the year.
PGY1 year is broken down as follows:
- 3 months of General Orthopaedics (James A. Haley VA Hospital)
- 3 months of Orthopaedic Trauma at a Level 1 Trauma Center (Tampa General Hospital)
- 1 month of dedicated Musculoskeletal Radiology (Moffitt Cancer Center)
- 5 months of General Surgery Training including 1 month each of Neurosurgery, Plastic Surgery, Vascular Surgery, General Surgery Trauma, and Surgical ICU
Rotation Level: PGY 2
The second year resident will be exposed to each individual orthopaedic surgical sub-specialty in the clinical and surgical setting. The diversity of this experience is invaluable, as residents participate in patient care through a busy private practice, an academic Level 1 Trauma Center, Ambulatory Surgery Centers, a nationally recognized Cancer Center, VA Hospital, and dedicated pediatric hospitals providing both bread-and-butter pediatric orthopaedic care and specialized deformity correction in a philanthropic model.
A prime focus of second year is to build upon the foundation that has been established. This early sub-specialty exposure permits understanding of the nuances and specifics of the differing fields within orthopaedic surgery, while continuing to build upon basic orthopaedic knowledge. The second year resident will enhance their surgical skills and dexterity under the direct tutelage of experienced, high-volume surgeons. Residents will become proficient in the indications, techniques, and surgical execution of total and partial joint arthroplasty, large and small joint arthroscopy, percutaneous and open fracture fixation, correction of spinal, long bone, and joint deformities, musculoskeletal oncology, and the reconstruction, augmentation, and/or transfer of ligaments, tendons, and/or nerves. Additionally, residents gain independence and autonomy through taking call at various hospitals throughout the year. This is invaluable to teach one how to manage the differing acuity of consults, stabilize traumatic injuries, communicate effectively with senior residents and attending surgeons, and understand and execute appropriate treatment plans for surgical and non-surgical care.
There is a protected Night Float / Research month with ample dedicated research coordinators, PhD statisticians, engineers, support staff, and departmental funding. This allows the second year resident to focus on study design, craft a protocol and IRB, collect and analyze data, and compose a manuscript. The goal of this initial research month is not to simply complete a project, but rather to gain familiarity with the scientific process and learn how to answer real and meaningful questions in orthopaedics.
PGY2 year is broken down as follows:
- 1 month of Musculoskeletal Oncology
- 1 month of Shoulder and Elbow Surgery
- 1 month of Adult Joint Reconstruction
- 1 month of Pediatric Orthopaedic Surgery
- 1 month of Sports
- 1 month of Spine Surgery
- 1 month of Foot and Ankle Surgery
- 1 month of General Orthopaedics
- 1 month of Hand and Upper Extremity Surgery
- 1 month of Orthopaedic Trauma
- 1 month of Pediatric Orthopaedic Surgery
- 1 month of Night Float / Research
Rotation Level: PGY 3
The third year resident begins the year armed with a strong foundation of basic orthopaedic surgical principles, an intensive year long immersion in the various sub-specialties, and an understanding of basic surgical techniques and execution. The expectation as the year progresses is for the third year resident to gain continued proficiency with pre-operative surgical planning, intra-operative surgical execution, and post-operative patient management and activity progression. Third year residents are further expected to assume greater responsibility in educating junior residents, and are also afforded greater autonomy as the year progresses.
Furthermore, third year residents continue developing research topics and advancing projects of interest throughout the year. Time and funding are afforded for regional and national conference presentation, as public speaking and academic achievement are vital in cultivating capable orthopaedic surgeons who will become leaders in the field.
PGY3 year is broken down as follows:
The third year is divided into 6 rotations of 2 months duration each. Of the 12 sub-specialty rotations during PGY2 year, six are repeated during PGY3 year and the remaining six are repeated during PGY4 year. Thus, all residents will rotate through every single orthopaedic surgical sub-specialty twice by the time they complete their PGY4 year. This affords repetition and additional exposure to the specifics of each sub-specialty. It allows increased surgical autonomy as a PGY3 and PGY4, as residents are already familiar with the individual sub-specialty services, hospitals, and surgical techniques from their PGY2 year.
Rotation Level: PGY 4
Fourth year continues to build upon the development seen in third year, with residents gaining additional surgical autonomy and understanding of more complex patient management. They complete the remaining 6 sub-specialty rotations (2 months duration each), as detailed above, and thus round out two complete passes through the entire breadth of orthopaedic surgical sub-specialties. Fourth year residents are expected to assume leadership roles within the residency and contribute to junior resident education.
A key element during the first half of PGY4 year is the preparation, application, and interviews for fellowship. The ability to rotate and experience each of the orthopaedic surgical sub-specialties in PGY2 is critical to identify one’s area of interest early on. This permits further exploration of this as a possible career choice during PGY3 and PGY4 year, develop mentor relationships within a potential field of interest, and tailor one’s research initiatives towards a sub-specialty interest. Thus, PGY4 residents are well prepared for fellowship applications with strong recommendation letters from mentors, valuable research experiences, and a genuine understanding and interest in that particular area that was cultivated through early exposure.
Similar to the more junior years, fourth year residents also participate in year long cadaveric anatomy sessions and skills labs to solidify surgical execution, practice more rare or subtle surgical scenarios, and become familiar with less common instrumentation. PGY residents are expected to adopt a stronger leadership and guidance role to junior residents.
Rotation Level: PGY 5
The chief resident has built upon the initial foundation, mastering basic orthopaedic principles. They have had multiple exposures to all orthopaedic sub-specialties and have managed patients on services in a variety of clinical and surgical settings. The prime goal of chief year is to serve as a capstone, solidifying more advanced orthopaedic surgical techniques. The ability to operate with autonomy is not only allowed, but is expected. Chief residents lead the inpatient teams at the larger hospitals, guiding junior residents to ensure that all patients have appropriate treatment plans. They engage with chiefs and attendings of other inpatient services to collaborate and dictate appropriate, timely inter-disciplinary patient care. Chiefs are expected to educate junior residents regarding patient evaluation and management, provisional reduction and stabilization, and guide junior residents through level-appropriate surgical cases. Fifth year residents guide junior residents in appropriate dissection and surgical approach techniques.
The importance of leadership is strongly emphasized, and dedicated lectures and meetings are scheduled with mentoring attending surgeons, the Residency Program Director, and Department Chairman. The business of orthopaedic surgical practice is strongly emphasized, and guidance and advice are provided during the evaluation of potential employment opportunities. Further career development opportunities are available, with time and funding provided to pursue regional, national, or international conferences of interest.
PGY5 year is broken down as follow:
- 3 months of General Orthopaedics
- 3 months of Orthopaedic Trauma
- 3 months of Hand and Upper Extremity Surgery
- 3 months of Orthopaedic Trauma and Adult Joint Reconstruction
Orthopaedic Surgery Milestones & Core Competencies
The University of South Florida & Florida Orthopaedic Institute Orthopaedic Surgery Residency Program strives to train exceptional orthopaedic surgeons and physicians, and adheres to the Orthopaedic Surgery Milestones and Core Competencies set forth by the ACGME (Accreditation Council for Graduate Medical Education) and the ABOS (American Board of Orthopaedic Surgery).
These are freely available through the ACGME and ABOSwebsite:
https://www.acgme.org/Specialties/Milestones/pfcatid/14/Orthopaedic
https://www.abos.org/residency-programs